1. World Health Organization. Traditional Medicine. Geneva:World Health Organization;2003. Available from:http//www.who/m/medical/centre/factsheet/ts/34/en/pirria/html. [Last accessed on 2020 Nov 22].
2. Mann A, Amupitan JO, Oyewale AO, Okogun JI, Ibrahim K. An ethnobotanical survey of indigenous flora for treating tuberculosis and other respiratory diseases in Niger State, Nigeria. J Phytomed Ther 2007;12:1-12.
3. Anyamene CO, Ezeadila JO. Antibacterial activity of water, ethanol and methanol extracts of Ocimum gratissimum, Vernonia amygdalina and Afromomum melegueta. J Appl Sci 2010;13:8940-8.
4. Sasidharan S, Chen Y, Saravanan D, Sundram KM, Latha LY. Extraction, isolation and characterization of bioactive compounds from plants'extracts. Afr J Tradit Complement Altern Med 2011;8:1-101.
5. Ogbulie JN, Ogueke CC, Nwanebu FC. Antibacterial properties of Uvaria chamae, Congronema latifolium, Garcinia kola, Vemonia amygdalina and Aframomium melegueta. Afr J Biotechnol 2007;6:1549-53.
6. Prince L, Prabakaran P. Antifungal activity of medicinal plants against plant pathogenic fungus Colletotrichum falcatum. Asian J Plant Sci Res 2011;1:84-7.
7. Hennenberg KJ, Geotze V, Minden DT, Porembsk S. Size-class distribution of Anogeissus leiocarpa (Combretaceae) along forest savannah ecotones in Northern Ivory coast. J Trop Ecol 2005;21:273-81.
8. Victor YA. In vitro assessment of antioxidant and antimicrobial activities of methanol extracts of six wound healing medicinal plants. J Nat Sci Res 2013;3:74-82.
9. Owoseni AA, Ogunnusi T. Antibacterial effect three selected chewing sticks extracts on Lactobacillus spp. Into J Trop Med 2006;3:103.
10. Kwame TA, Stephen KW, Anthony FK, Jeffery W. Finora A. Compositions Comprising Natural Agent for the Treatment of HIV-Associated Opportunities Infection and Complication and Method for Prepating and Using Composition Comprising Natural Agents;2005. Available from:http://www.freepalentsonline.comly2005/0266105. [Last accessed on 2018 Oct 12].
11. Taiwo O, Xu H, Lee S. Antibacterial activities of extracts from Nigerian chewing sticks. Phytother Res 1999;13:675-9.
12. Onyeyili PA. Anthelminthic Efficacy of Some Plants used in Ethnoveterinary Practices in the Arid Zone of North Eastern Nigeria RGA No. 28, Project Report;2000. 21.
13. Amin OM. Perspectives on gastro-intestinal pathogenic bacteria infections in humans. EC Microbiol 2019;15:1173-85.
14. Rosenberger CM, Scott MG, Gold MR, Hancock RE, Finley, RB. Salmonella typhimurium infection and lipopolysaccharide stimulation induce similar changes in macrophage gene expression. J Immunol 2000;164:5894-904.
15. Yasin N, Jabeen A, Nisa I, Tasleem U, Khan H, Shah FM, et al. A review:Typhoid fever. J Bacteriol Infect Dis 2018;2:1-7.
16. Hancock EW. Mechanisms of action of never antibiotic for gram-positive pathogens Lancet Infect Dis 2005;5:209-18.
17. Salih RR, Gibreel HH, Ahmed DM, Hammad ZM, Ahmed AI. Antimicrobial effect of aqueous and ethanolic leaves extracts of Ziziphus species against animal bacterial pathogens. Curr Trends For Res2019;3:1-6.
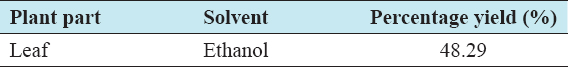
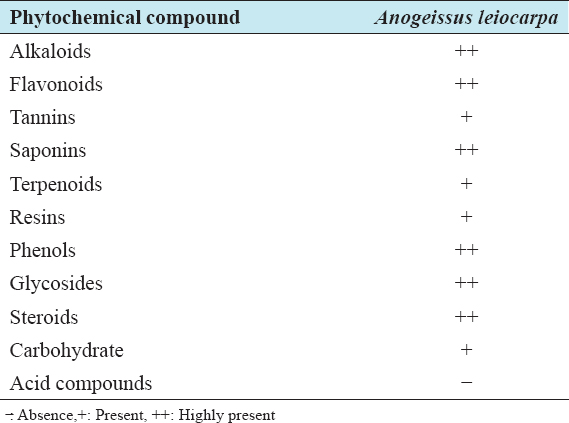
18. Chomini MS, Peter MK, Ameh M, Chomini AE, Bassey EA, Ayodele AO. Phytochemical Screening and Antibacterial Activities of Aframomum melegueta (K. Schum) Seed Extracts on Salmonella typhi and Klebsiella pneumoniae. JAppl Sci Environ Manage 2020;24:1419-24.
19. Ncube NS, Afolayan AJ, Okoh AI. Assessment techniques of antimicrobial properties of natural compounds of plant origin:Current methods and future trends. Afr J Biotechnol 2008;7:1797-806.
20. Ardzard SS, Yusuf AA, Muhammed M, David S, Odugba M, Okwon AE. Combine antibacterial effect of Moringa oleifera leaves extract and honey on some bacteria associated with wounds and gastroenteritis. J Adv Med Pharm Sci 2009;3:16-23.
21. Parekh J, Jadeja D, Chanda S. Efficacy of aqueous and methanol extracts of some medicinal plants for potential antibacterial activity. Turk J Biol 2005;29:203-10.
22. Ikeyi A, Ogbonna A, Eze F. Phytochemical analysis of paw-paw (Carica papaya) leaves. Int J Life Sci Biotechnol Pharm Res 2013;2:347-51.
23. Ghamba PE, Balla H, Goje LJ, Halidu A, Dauda MD. In vitro antimicrobial activities of Vernonia amygdalina on selected clinical isolates. Int J Curr Microbiol Appl Sci 2014;3:1103-13.
24. Akimnibosun HA, Akinnibosun FI, Adieme BC. Bio therapeutic potential of aqueous an ethanol extracts of leaves on some vegetable gram negative bacteria. Bot Environ Sci JTrop2009;6:3337.
25. Cheesbrough M. Antibacterial Sensitive Affecting. District Laboratory Practice in Tropical Counties, Part 2. Cape Town, South Africa:Cambridge University Press;2000. 132-43.
26. Cheruiyot KR, Olila D, Kateregga J. In vitro antibacterial activity of selected medicinal plants from Longisa region of Bomet district. Kenya Afr Health Sci 2009;9:542-6.
27. Nweze EI, Okafor JI, Njoku O. Antimicrobial activities of methanolic extracts of Trema guineensis (Schumm and Thorn) and Morinda lucida Benth used in Nigerian herbal medicinal practice. J Biol Res Biotechnol 2004;2:39-46.
28. Edeoga HO, Okwu DE, Mbaebie BO. Phytochemical constituents of some Nigerian medicinal plants. Afr J Biotechnol 2005;4:685-8.
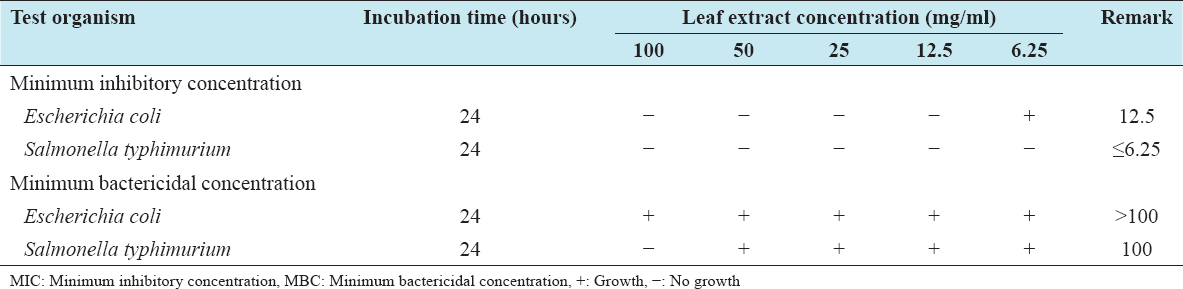
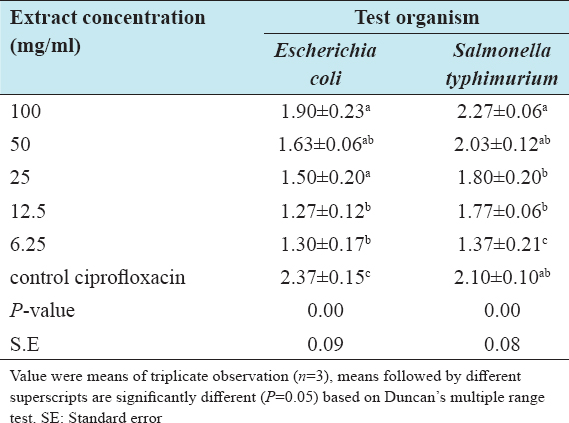
29. Zumbes HJ, Belenu TO, Onwuliri FC. In vitro antibacterial activity of Anogeissus leiocarpa leaf extracts on some bacteria associated with diarrhea. Int J Nat Appl Sci 2007;3:53-6.
30. Ogundana OT, Gunlaria O, Farombi OE. Morindalucida;antionidant and reducing activities of crude methanolic stem bark extracts. Adv Nat Appl Sci 2008;2:49-54.
31. Nwinyi OC, Chinedu NS, Ajani OO. Evaluation of antibacterial activities of Pisidum guajava and Gongronema latifolium. J Med Plant Res 2008;2:189-92.
32. Adejumobi JA, Ogundiya MO, Kolapo AL, Okunada MB. Phytochemical composition and in vitro antimicrobial activity of Anogeissus leiocarpa on some common oval pathogen. J Med Plants Res 2008;2:193-6.
33. Mann A. Evaluation of antimicrobial activity of Anogeissus leiocarpus and Terminalia auicenniodes against infection diseases prevelent in Hospital environment in Nigeria. J Microbiol Res 2012;2:6-1.
34. Timothy SY, Mashi FI, Helga BI, Galadima IH, Midala TA. Phytochemical screening, antibacterial evaluation and in vitro spasmodic effect of the aqueous and ethanol leaf and stem bark extracts of Anogeissus leiocarpus (DC) Guill and Perr. Asian J Pharm Sci Technol 2015;5:302-8.
35. Umar HY, Muhammad AI. Antibacterial activities of leaves extract of Anogeissus leiocarpa and Vitex doniana against some bacteria. Am J Innov Res Appl Sci 2015;1:384-8.
36. Bereksi MS, Hassaïne H, Bekhechi C, Abdelouahid DE. Evaluation of antibacterial activity of some medicinal plants extracts commonly used in Algerian traditional medicine against some pathogenic bacteria. Pharmacogn J 2018;10:507-12.