1. Kumar R, Lu SK, Minchom A, Sharp A, Davidson M, Gunapala R, et al. A phase 1b trial of the combination of an all-oral regimen of capecitabine and erlotinib in advanced non-small cell lung cancer in Caucasian patients. Cancer Chemother Pharmacol 2016;77:375-83.
2. Falzone L, Salomone S, Libra M. Evolution of cancer pharmacological treatments at the turn of the third millennium. Front Pharmacol 2018;9:1300.
3. Blum HE. Hepatocellular carcinoma:Therapy and prevention. World J Gastroenterol 2005;11:7391-400.
4. Luo D, Carter KA, Miranda D, Lovell JF. Chemophototherapy:An emerging treatment option for solid tumors. Adv Sci (Weinh) 2016;4:1600106.
5. Jin J, Chen J, Suo S, Qian W, Meng H, Mai W, et al. Low-dose cytarabine, aclarubicin and granulocyte colony-stimulating factor priming regimen versus idarubicin plus cytarabine regimen as induction therapy for older patients with acute myeloid leukemia. Leuk Lymphoma 2015;56:1691-7.
6. Szwed M, Laroche-Clary A, Robert J, Jozwiak Z. Efficacy of doxorubicin-transferrin conjugate in apoptosis induction in human leukemia cells through reactive oxygen species generation. Cell Oncol (Dordr) 2016;39:107-18.
7. Chow R, Tsao M, Chiu L, Popovic M, Milakovic M, Lam H, et al. Efficacy of the combination neurokinin-1 receptor antagonist, palonosetron, and dexamethasone compared to others for the prophylaxis of chemotherapy-induced nausea and vomiting:A systematic review and meta-analysis of randomized controlled trials. Ann Palliat Med 2018;7:221-33.
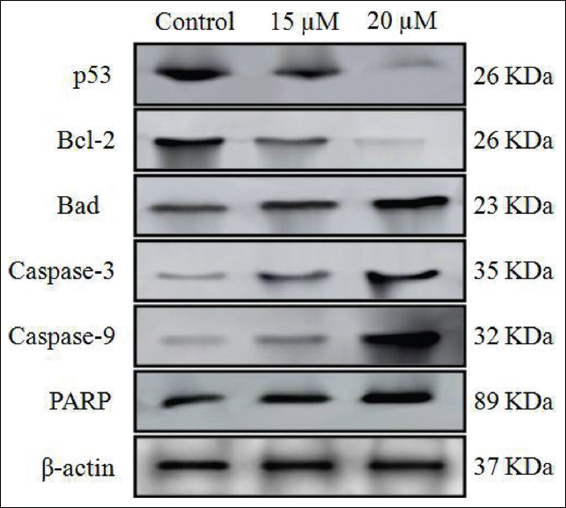
8. Hail N Jr., Carter BZ, Konopleva M, Andreeff M. Apoptosis effector mechanisms:A requiem performed in different keys. Apoptosis 2006;11:889-904.
9. Abraham MC, Shaham S. Death without caspases, caspases without death. Trends Cell Biol 2004;14:184-93.
10. Halliwell B. Oxidative stress in cell culture:An under-appreciated problem?FEBS Lett 2003;5403-6.
11. Ozben T. Oxidative stress and apoptosis:Impact on cancer therapy. J Pharm Sci 2007;96:2181-96.
12. Dey D, Das S, Yadav R, Ranjani A, Gyathri L, Roy SC, et al. Design of a mononuclear copper (II)-phenanthroline complex:Catechol oxidation, DNA cleavage and antitumor properties. Polyhedron 2016;106:106-14.
13. Lee KH. Discovery and development of natural product-derived chemotherapeutic agents based on a medicinal chemistry approach. J Nat Prod 2010;73:500-16.
14. Remila S, Atmani-Kilani D, Delemasure S, Connat J, Azib L. Antioxidant cytoprotective, anti-inflammatory and anticancer activities of Pistacia lentiscus (Anacardiaceae) leaf and fruit extracts. Eur J Integr Med 2015;7:274-86.
15. Newman DJ, Cragg GM, Snader KM. Natural products as sources of new drugs over the period 1981-2002. J Nat Prod 2003;66:1022-37.
16. Paik SY, Koh KH, Beak SM, Paek SH, Kim JA. The essential oils from Zanthoxylum schinifolium pericarp induce apoptosis of HepG2 human hepatoma cells through increased production of reactive oxygen species. Biol Pharm Bull 2005;28:802-7.
17. Vernin GA, Parkanyi C, Cozzolino F, Fellous R. GC/MS Analysis of the Volatile Constituents of Corymbia citriodora Hook. From Réunion Island. J Essent Oil Res 2004;16:560-5.
18. Bounihi A, Hajjaj G, Alnamer R, Cherrah Y, Zellou A. In vivo potential anti-inflammatory activity of Melissa officinalis L. essential oil. Adv Pharmacol Sci 2013;2013:101759.
19. Rao BR, Kaul PN, Syamasundar KV, Ramesh S. Comparative composition of decanted and recovered essential oils of Eucalyptus citriodora Hook. Flavour Fragr J 2003;18:133-5.
20. Silva MI, Silva MA, de Aquino Neto MR, Moura BA, de Sousa HL, de Lavor EP, et al. Effects of isopulegol on pentylenetetrazol-induced convulsions in mice:Possible involvement of GABAergic system and antioxidant activity. Fitoterapia 2009;80:506-13.
21. Dias LD, de Carvalho AL, Pinto SM, Aquino GL, Calvete MJ, Rossi LM, et al. Bioinspired-metalloporphyrin magnetic nanocomposite as a reusable catalyst for synthesis of diastereomeric (-)-isopulegol epoxide:Anticancer activity against human osteosarcoma cells (MG-63). Molecules 2018;24:52.
22. Silva MI, Moura BA, Neto MR, ToméAda R, Rocha NF, de Carvalho AM, et al. Gastroprotective activity of isopulegol on experimentally induced gastric lesions in mice:Investigation of possible mechanisms of action. Naunyn Schmiedebergs Arch Pharmacol 2009;380:233-45.
23. Próspero DF, Filho AC, Piauilino CA, Lopes EM, de Sousa DP, de Castro Almeida FR. Effects of isopulegol in acute nociception in mice:Possible involvement of muscarinic receptors, opioid system and l-arginine/NO/cGMP pathway. Chem Biol Interact 2018;293:55-60.
24. Oliveira Fde A, Andrade LN, de Sousa EB, de Sousa DP. Anti-ulcer activity of essential oil constituents. Molecules 2014;19:5717-47.
25. Ames BN, Mccann J, Yamasaki E. Methods for detecting carcinogens and mutagens with the Salmonella/mammalian-microsome mutagenicity test. Mutat Res 1975;31:347-64.
26. Mosmann T. Rapid colorimetric assay for cellular growth and survival:Application to proliferation and cytotoxicity assays. J Immunol Methods 1983;65:55-63.
27. Merlin NJ, Parthasarathy V, Santhoshkumar TR. Induction of apoptosis in huma breast cancer cell line MCF-7 by phytochemicals from Gmelina asiatica. Afr J Biotech 2010;9:4451-6.
28. Eskandani M, Hamishehkar H, Dolatabadi JE. Cytotoxicity and DNA damage properties of tert-butylhydroquinone (TBHQ) food additive. Food Chem 2004;153:315-20.
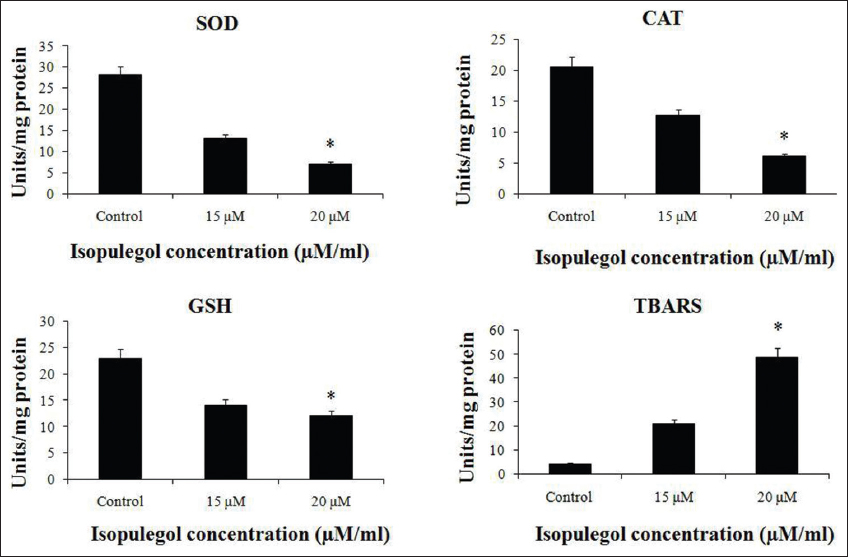
29. Sun YI, Oberley LW, Li Y. A simple method for clinical assay of superoxide dismutase. Clin Chem 1988;34:497-500.
30. Góth L. A simple method for determination of serum catalase activity and revision of reference range. Clin Chim Acta 1991;196:143-51.
31. Rotruck JT, Pope AL, Ganther HE, Swanson AB, Hafeman DG, Hoekstra WG. Selenium:Biochemical role as a component of glutathione peroxidase. Science 1973;179:588-90.
32. Buege JA, Aust SD. Microsomal lipid peroxidation. Methods Enzymol 1978;52:302-10.
33. Maucort-Boulch D, de Martel C, Franceschi S, Plummer M. Fraction and incidence of liver cancer attributable to hepatitis B and C viruses worldwide. Int J Cancer 2018;142:2471-7.
34. Cort A, Ozben T, Saso L, De Luca C, Korkina L. Redox control of multidrug resistance and its possible modulation by antioxidants. Oxid Med Cell Longev 2016;2016:4251912.
35. Shigematsu H, Yoshida K, Sanada Y, Osada S, Takahashi T, Wada Y, et al. Rapamycin enhances chemotherapy-induced cytotoxicity by inhibiting the expressions of TS and ERK in gastric cancer cells. Int J Cancer 2010;126:2716-25.
36. Saha SK, Sikdar S, Mukherjee A, Bhadra K, Boujedaini N, Khuda-Bukhsh AR. Ethanolic extract of the goldenseal, Hydrastis canadensis, has demonstrable chemopreventive effects on HeLa cells in vitro:Drug-DNA interaction with calf thymus DNA as target. Environ Toxicol Pharmacol 2013;36:202-14.
37. Ansil PN, Wills PJ, Varun R, Latha MS. Cytotoxic and apoptotic activities of Amorphophallus campanulatus (Roxb.) Bl. tuber extracts against human colon carcinoma cell line HCT-15. Saudi J Biol Sci 2014;21:524-31.
38. Peng CH, Huang CN, Hsu SP, Wang CJ. Penta-acetyl geniposide induce apoptosis in C6 glioma cells by modulating the activation of neutral sphingomyelinase-induced p75 nerve Growth factor receptor and protein kinase Cdelta pathway. Mol Pharmacol 2006;70:997-1004.
39. Niska K, Santos-Martinez MJ, Radomski MW, Inkielewicz-Stepniak I. CuO nanoparticles induce apoptosis by impairing the antioxidant defense and detoxification systems in the mouse hippocampal HT22 cell line:Protective effect of crocetin. Toxicol In Vitro 2015;29:663-71.
40. He L, He T, Farrar S, Ji L, Liu T, Ma X. Antioxidants maintain cellular redox homeostasis by elimination of reactive oxygen species. Cell Physiol Biochem 2015;44:532-53.
41. Gherghi IC, Girousi ST, Voulgaropoulos AN, Tzimou-Tsitouridou R. Study of interactions between DNA-ethidium bromide (EB) and DNA-acridine orange (AO), in solution, using hanging mercury drop electrode (HMDE). Talanta 2003;61:103-12.
42. Vandghanooni S, Forouharmehr A, Eskandani M, Barzegari A, Kafil V, Kashanian S, et al. Cytotoxicity and DNA fragmentation properties of butylated hydroxyanisole. DNA Cell Biol 2013;32:98-103.
43. Zhou GZ, Shi YY, Cui LS, Li AF, Wang QQ, Liu M. Oxymatrine induces A549 human non�small lung cancer cell apoptosis via extrinsic and intrinsic pathways. Mol Med Rep 2018;17:1071-6.
44. Dragovich T, Gordon M, Mendelson D, Wong L, Modiano M, Chow HH, et al. Phase I trial of imexon in patients with advanced malignancy. J Clin Oncol 2007;25:1779-84.
45. Alexandre J, Nicco C, Chéreau C, Laurent A, Weill B, Goldwasser F, et al. Improvement of the therapeutic index of anticancer drugs by the superoxide dismutase mimic mangafodipir. J Natl Cancer Inst 2006;98:236-44.
46. Xiao D, Powolny AA, Moura MB, Kelley EE, Bommareddy A, Kim SH, et al. Phenethyl isothiocyanate inhibits oxidative phosphorylation to trigger reactive oxygen species-mediated death of human prostate cancer cells. J Biol Chem 2010;285:26558-69.
47. Das L, Vinayak M. Long term effect of curcumin in restoration of tumour suppressor p53 and phase-II antioxidant enzymes via activation of Nrf2 signalling and modulation of inflammation in prevention of cancer. PLoS One 2015;10:e0124000.
48. Gong Z, Yang Q, Zeng Z, Zhang W, Li X, Zu X, et al. An integrative transcriptomic analysis reveals p53 regulated miRNA, mRNA, and lncRNA networks in nasopharyngeal carcinoma. Tumour Biol 2013;37:3683-95.
49. Villa-Pulgarín JA, Gajate C, Botet J, Jimenez A, Justies N, Varela M, et al. Mitochondria and lipid raft-located FOF1-ATP synthase as major therapeutic targets in the antileishmanial and anticancer activities of ether lipid edelfosine. PLoS Negl Trop Dis 2017;11:e0005805.
50. Bao H, Zhang Q, Zhu Z, Xu H, Ding F, Wang M, et al. BHX, a novel pyrazoline derivative, inhibits breast cancer cell invasion by reversing the epithelial-mesenchymal transition and down-regulating Wnt/b-catenin signalling. Sci Rep 2017;7:9153.
51. Shang HS, Chang CH, Chou YR, Yeh MY, Au MK, Lu HF, et al. Curcumin causes DNA damage and affects associated protein expression in HeLa human cervical cancer cells. Oncol Rep 2016;36:2207-15.
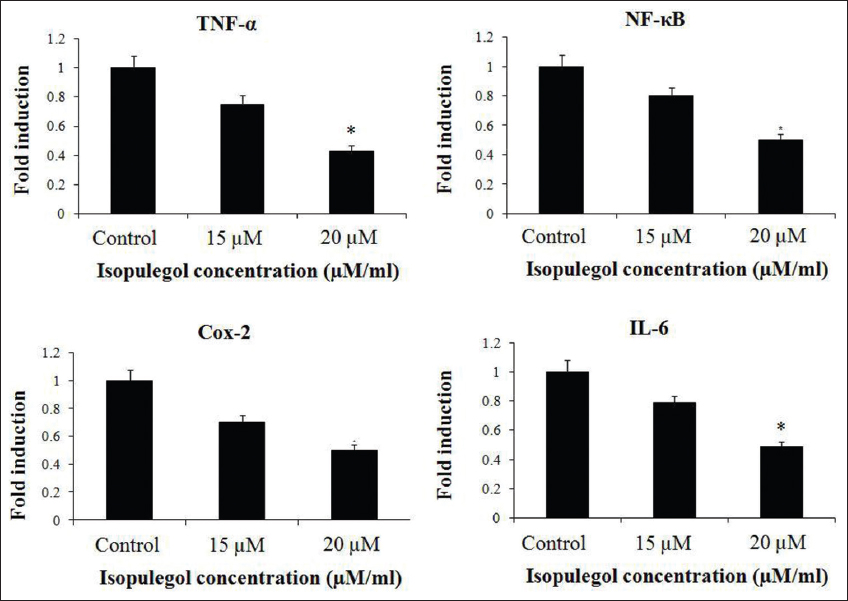
52. Yang HJ, Wang M, Wang L, Cheng BF, Lin XY, Feng ZW. NF-kB regulates caspase-4 expression and sensitizes neuroblastoma cells to Fas-induced apoptosis. PLoS One 2015;10:e0117953.
53. Zheng HC. The molecular mechanisms of chemoresistance in cancers. Oncotarget 2017;8:59950-64.